As part of a five-month operation theatre overhaul at a trust hospital, I, Dr. Shantanu Gulati, have closely engaged with several critical aspects of surgical infrastructure—including autoclaves. This blog is an effort to document and share real, on-ground learnings through facts, images, and videos that may help other ophthalmologists facing similar decisions.
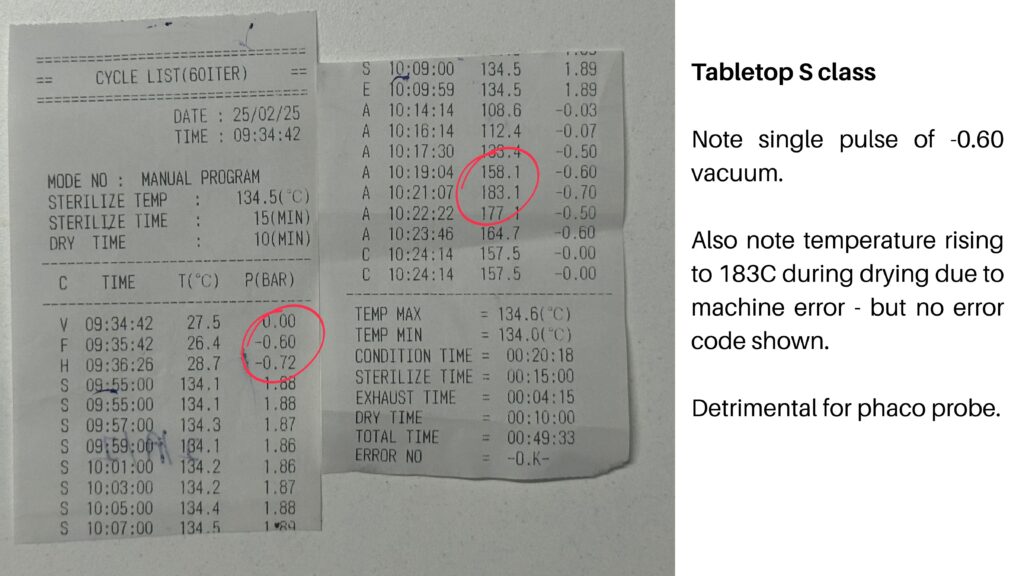
I do not claim to be a technical expert. My objective is to bridge the gap between the clinical perspective of an ophthalmologist and the technical complexities of sterilization equipment. Most of my experience is with Medister autoclaves, and therefore, the discussion throughout this blog will be framed in that context. Inputs from fellow ophthalmologists are most welcome and will be carefully vetted and added in continuity.
Before we dive in, here’s why you can trust this guide.
Based on my experience during this OT overhaul, I was invited to present on “Modular OT Features” at the UPSOS Practice Enhancement Series webinar. In the same session, Dr. Mathew Kurian delivered an excellent, in-depth presentation on autoclaving and sterilization protocols.
While his talk focused on the technical and microbiological aspects, this blog serves as a practical, on-ground buying guide — shaped by real decisions we faced while planning OT infrastructure.
🎥 The full webinar clip is embedded below for your reference.
1. First Things First: How Does Steam Sterilize?
At its core, steam sterilization is about heat transfer. Steam carries latent heat that, when transferred to microorganisms, disrupts proteins and effectively kills them. You would have heard 121C at 1bar for 20 minutes or 134C at 2 bar for 7 minutes. So a scientifically derived temperature is required to be maintained in direct contact with all surfaces of the items to be sterilised at a high pressure that helps achieve the said temperature faster and promotes steam penetration.
While temperature, pressure and time duration are commonly spoken about and generally understood well by our community, what is often neglected is that the sterilization process only works if steam comes in direct contact with all surfaces. That means contact time is just as critical—if not more—than just the total cycle duration.
Temperature benchmarks like 121°C for 15–30 minutes or 134°C for shorter cycles are based on the assumption that saturated steam has direct access to the instruments. But this doesn’t happen automatically. For steam to sterilize effectively, it must physically displace the air already present in the chamber and within the lumens of instruments. Without this displacement, you’re left with air pockets, and steam simply cannot sterilize through air.
2. Out With the Air: Gravity vs. Pre-Vacuum Systems
Air displacement is the single biggest barrier to effective steam sterilization. There are two main ways autoclaves attempt this: gravity displacement and pre-vacuum systems.
In gravity-based systems, steam enters the chamber from the top or side and pushes air downward and out through a drain at the bottom. This method is slow, inefficient, and often incomplete—especially when it comes to ophthalmic instruments with narrow lumens, like phaco handpieces, vitrectomy cutters, and cannulas. Air tends to get trapped in these spaces, creating sterile-looking but non-sterile realities.
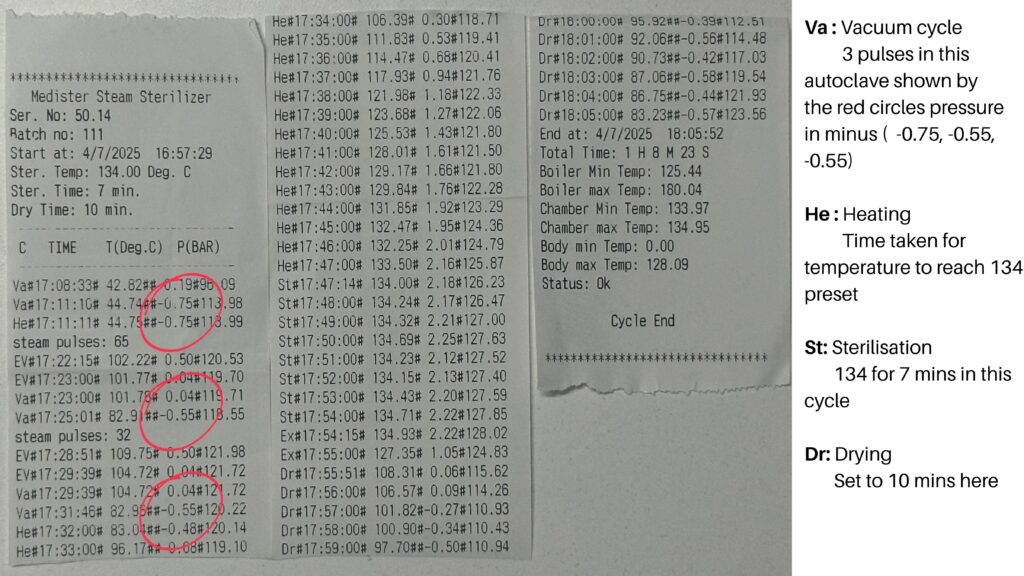
Modern pre-vacuum (or Class B) systems solve this by using a vacuum pump to actively evacuate air from the chamber before introducing steam. This ensures steam reaches even the innermost parts of complex instruments and reduces the risk of air pockets. In 2025, for a specialty like ophthalmology that depends on high-precision, lumen-rich tools, gravity-based autoclaves are functionally obsolete.
The difficulty in removing air from narrow, long lumens is governed by principles of fluid dynamics—specifically Hagen–Poiseuille’s law, which states that resistance to flow increases exponentially as the diameter decreases and length increases. In practical terms, this means that the longer and narrower a lumen is, the harder it becomes to evacuate air from it. This creates a serious challenge for gravity-based sterilizers, as trapped air prevents steam from making direct contact with internal surfaces, compromising sterilization.
3. The Autoclave Class System : Class N / S /B
Autoclaves are broadly categorized into three types: N, S, and B. These classifications define how air is removed and how effective the sterilization process is, especially for wrapped, hollow, or lumen-containing instruments like those used in ophthalmology.
The table below outlines the fundamental differences:
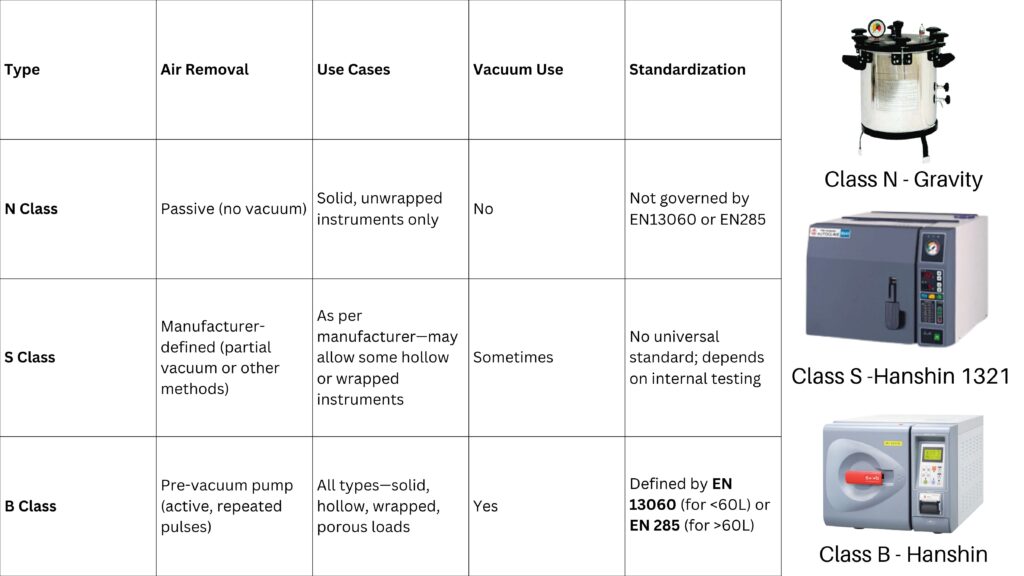
The definition of a true B Class autoclave comes from adherence to these specific standards:
- EN 13060 for benchtop autoclaves (chambers < 60L)
- EN 285 for larger, hospital-grade autoclaves
These standards dictate how many vacuum pulses, how deep the vacuum must reach, and how cycle performance is tested and validated.
During literature review and vendor interactions, full access to these PDFs (EN 13060 or EN 285) was not found publicly, and even if obtained, their technical content may be difficult for most of us to interpret in depth. That said, what is clear and critical is this:
If your autoclave is under 60L, a manufacturer’s declaration that the machine conforms to EN 13060 is the best assurance that it truly qualifies as a Class B.
For machines larger than 60L, EN 285 is the applicable benchmark.
Always ask for certification documentation that explicitly confirms this compliance. It’s the only way to rest assured that the “B Class” label isn’t just a marketing term.
4. The Shape of Sterilisation: Vertical, Horizontal, Manual, and More
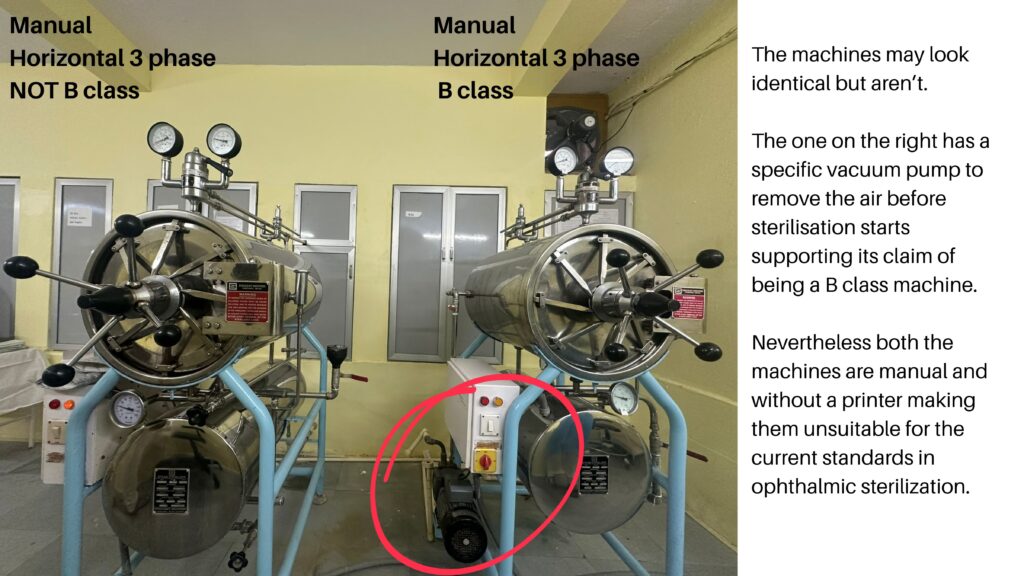
When selecting an autoclave, form factor and automation level are just as important as class. The terms vertical, horizontal, tabletop, manual, and automated often come up—but not all of them are suitable for surgical use, especially in ophthalmology.
Manual vs. Automated :
Any time of autoclave can be manual or automated, regardless of shape, size and class.
| Feature | Manual Autoclave | Automated Autoclave |
|---|---|---|
| Cycle Control | Manual shifting between stages | Microprocessor-controlled automatic cycles |
| Error Detection | Absent | Built-in error codes and fault detection |
| Parameter Validation | Not ensured | Sensors verify temperature and holding time |
| Printout/Documentation | Not available | Integrated printer provides sterilization logs |
| Compliance with NABH/Legal | Difficult to validate | Meets documentation needs for audits and medico-legal proof |
| Suitability for Ophthalmology | Not recommended | Strongly recommended |
| Status in Modern Practice | Obsolete | Current standard |
So the first thing to strive for in today’s day and age of documentation – is to an automated autoclave with a printer.
Vertical Autoclaves:
Vertical autoclaves are mostly gravity-based, with steam entering from the top and displacing air downward. They are not available in true B class form, despite occasional manufacturer claims of “vacuum.” In most vertical systems, this so-called vacuum refers only to a post-sterilization drying cycle, not pre-vacuum air removal. As a result, these autoclaves often leave wet loads and fall into the Class N category. For ophthalmic use, they are not recommended.

Vertical autoclaves are mostly used in setups where space is a constraint, or in places where a B class unit is available (albeit of a smaller size) that takes care of the instrument load and as such the vertical unit is used for the linen load.
Horizontal Autoclaves:
Horizontal autoclaves are available in both
- Tabletop sizes (<60L)
- Larger, floor-standing units (>60L).
| Parameter | Tabletop Autoclave | Floor-Standing Autoclave |
|---|---|---|
| Class Type | Can be B or S class | Can be B or S class |
| Chamber Size | Typically smaller. but can hold drums (e.g., Medister 50L holds two 11″ drums) | Usually larger; easily holds multiple large drums |
| Use Case | Suitable for Ophthalmology setups with 10-15 OTs/day | Suitable for super high-volume, multi-theatre, or hospital-wide setups |
| Automation | Mostly automated with microprocessor controls | May be manual or automated, depending on model |
| Space Requirement | Compact; requires less space | Requires dedicated floor space |
| Power Supply | Single-phase | Three-phase |
| Vacuum System | Diaphragm vacuum pump (no continuous water needed) | Water-ring vacuum pump (requires continuous water inlet) |
| Maintenance Analogy | Like a laptop – compact, efficient, but more delicate | Like a desktop – robust, lower maintenance, more scalable |
| Cost & Serviceability | Generally more expensive per liter of capacity; parts delicate | More economical per liter; parts easier to service |

5. Power backup for your autoclave
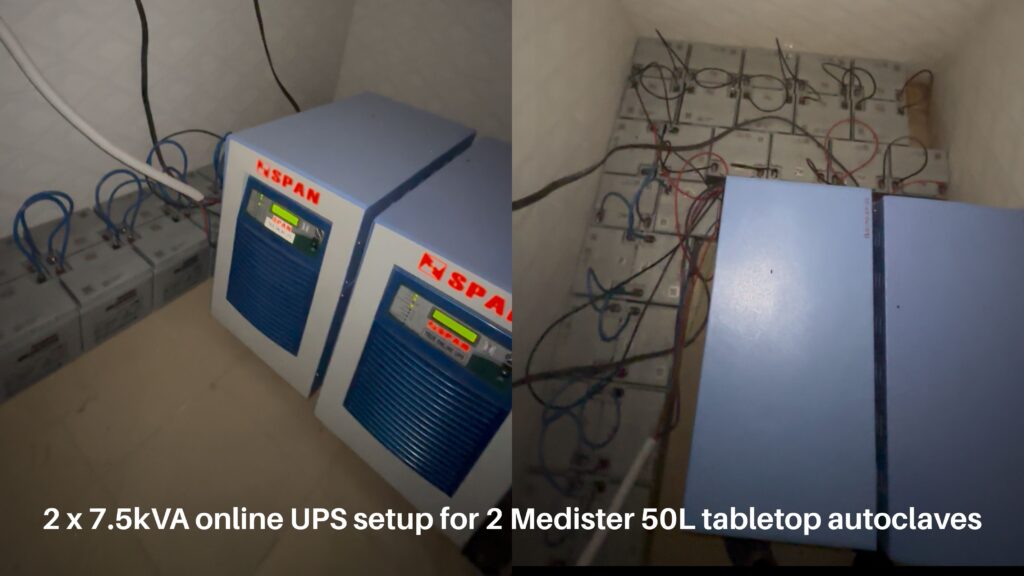
A topic of increasing importance with accreditations and inspections on the rise is o ensure uninterrupted power supply to the heart of the OT. Reliable power back ups to provide uninterrupted sterilization cycles and protect sensitive electronics are quickly becoming the norm and could be heavy on the pocket.
For a 4.5 kW autoclave, it is recommended to install an online UPS system of at least 7 kVA capacity. An online UPS provides consistent power without switching delays, protecting the machine from voltage fluctuations, surges, and sudden outages. The system should be backed by adequate battery backup—typically 30 to 60 minutes, depending on your load and workflow needs—to allow completion of ongoing sterilization cycles during a power cut. Ensure the UPS is properly grounded and regularly maintained to avoid equipment damage and ensure patient safety.
6. Boiling it down – Summary in a vacuum
- What is class N/S/B, vertical/horizontal, tabletop/standalone?
- None of it matters, you need one “automated – true class B” autoclave as described above – which is only available in horizontal form be it tabletop or standalone.
- So should I get a tabletop or standalone?
- Depends on your case load, the space available in your setup, and the electricity backup requirements you can afford.
- By design large standalone autoclaves are more efficient, use larger vacuum pumps of the wet type, are easier to maintain and cheaper, but require more space and higher kV and 3phase supply.
- Tabletop autoclaves are less efficient by design, more sensitive, more expensive but utilise less electricity and take lesser space.
- I dont have much space, can I not get a vertical autoclave at all?
- You can but only for linen and supportive paraphernalia, for instruments specially with lumens – Class B is the way to go.
- The smaller class B of 21L take lesser space than a small oven.
- So should I get an indian made autoclave or a korean/german machine?
- As long as you’re getting what you’re asking for truly – a true class B machine, either should work fine.
- But do remember you get what you pay for, there is a definite and clear difference between these machines, whether that difference is worth it to your practice depends on your budget. I have seen certain Indian brands being opened up for certain service requirements that arose solely due to poor part quality.
Thanks for scrubbing in till the end — may your instruments be sterile and your outcomes sparkling.
Inputs from fellow ophthalmologists are most welcome and will be carefully vetted and added in continuity.
